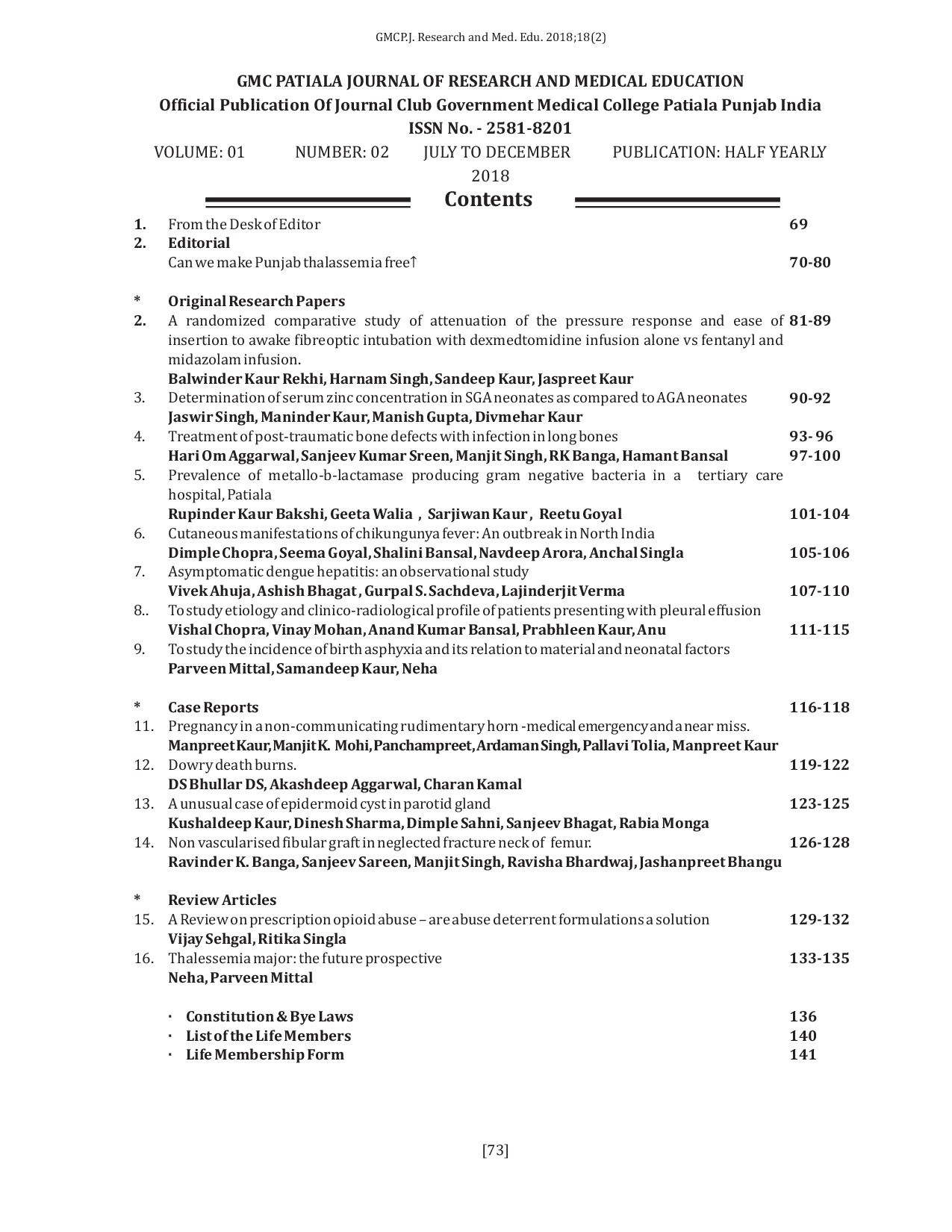
Treatment of Post-traumatic Bone Defects with Infection in Long Bones
Keywords:
Bone reconstruction,, Bone defect, Induced membrane, Open fracture, Bone infection,, Posttraumatic infected non unionAbstract
Masquelet technique, which is the use of a temporary cement spacer followed by staged bone grafting, is a recent treatment strategy to manage an infected nonunion with bone defect. This paper describes a series of 20 patients treated with this technique of staged bone grafting following placement of an antibiotic spacer to successfully manage infection as well as bone defects in long bones. The injured limbs were stabilized and aligned at the time of initial spacer placement. In our series, osseous consolidation was successfully achieved in all cases. This technique gives promising result in the management of post-traumatic bone defects associated with infection.
Downloads
References
A. Paige Whittle, “Fractures of the Lower Extremity,” In: S. Terry Canale and H. B. James, Eds., Campbell's Operative Orthopaedics, Mosby, Philadelphia, 2008, pp.3117-3146. [Citation Time(s):2]
J. T. Watson, M. Anders, and B. R. Moed, “Management strategies for bone loss in tibial shaft fractures,” Clinical Orthopaedics and Related Research, no. 315, pp. 138–152, 1995
H. Weinberg, V. G. Roth, G. C. Robin, and Y. Floman, “Early fibular bypass procedures (tibiofibular synostosis) for massive bone loss in war injuries,” Journal of Trauma, vol. 19, no. 3, pp. 177–181, 1979.
R. Hertel, A. Gerber, U. Schlegel, J. Cordey, P. Ruegsegger, and B. A. Rahn, “Cancellous bone graft for skeletal reconstruction: muscular versus periosteal bed—preliminary report,” Injury, vol. 25, supplement 1, pp. A59–A70, 1994.
A. C. Masquelet , “Muscle reconstruction in reconstructive surgery: soft tissue repair and long bone reconstruction,” Langenbeck's Archives of Surgery, vol. 388, no. 5, pp. 344–346, 2003.
A. C. Masquelet and T. Begue, “The concept of induced membrane for reconstruction of long bone defects,” Orthopedic Clinics of North America, vol. 41, no. 1, pp. 27–37, 2010.
A. C. Masquelet, F. Fitoussi, T. Begue, and G. P. Muller, “Reconstruction of the long bones by the induced membrane and spongy autograft,” Annales de Chirurgie Plastique et Esthetique, vol. 45, no. 3, pp. 346–353, 2000.
T. A. McCall, D. S. Brokaw, B. A. Jelen et al., “Treatment of large segmental bone defects with reamer-irrigatoraspirator bone graft: technique and case series,” Orthopedic Clinics of North America, vol. 41, no. 1, pp. 63–73, 2010
C. Y.-L. Woon, K.-W. Chong, and M.-K. Wong, “Induced membranes—a staged technique of bone-grafting for segmental bone loss. A report of two cases and a literature review,” The Journal of Bone and Joint Surgery. American, vol. 92, no. 1, pp. 196–201, 2010.
P. Pelissier, A. C. Masquelet, R. Bareille, S. M. Pelissier, and J. Amedee, “Induced membranes secrete growth factors including vascular and osteoinductive factors and could stimulate bone regeneration,” Journal of Orthopaedic Research, vol. 22, no. 1, pp. 73–79, 2004.1. V. Viateau, G. Guillemin, Y. Calando et al., “Induction of a barrier membrane to facilitate reconstruction of massive segmental diaphyseal bone defects: an ovine model,” Veterinary Surgery, vol. 35, no. 5, pp. 445–452, 2006.
O. M. Aho, P. Lehenkari, J. Ristiniemi, S. Lehtonen, J. Risteli, and H. V. Leskela, “The mechanism of action of induced membranes in bone repair,” The Journal of Bone and Joint Surgery. American, vol. 95, no. 7, pp. 597–604, 2013.
D. J. Biau, S. Pannier, A. C. Masquelet, and C. Glorion, “Case report: reconstruction of a 16-cm diaphyseal defect after Ewing's resection in a child,” Clinical Orthopaedics and Related Research, vol. 467, no. 2, pp. 572–577, 2009.
F. Accadbled, P. Mazeau, F. Chotel, J. Cottalorda, J. Sales de Gauzy, and R. Kohler, “Induced-membrane femur reconstruction after resection of bone malignancies: three cases of massive graft resorption in children,” Orthopaedics & Traumatology, Surgery & Research, vol. 99, no. 4, pp. 479–483, 2013.
N. T. O'Malley and S. L. Kates, “Advances on the Masquelet technique using a cage and nail construct,” Archives of Orthopaedic and Trauma Surgery, vol. 132, no. 2, pp. 245–248, 2012.
L. K. Huffman, J. G. Harris, and M. Suk, “Using the bimasquelet technique and reamer-irrigator-aspirator for post-traumatic foot reconstruction,” Foot and Ankle International, vol. 30, no. 9, pp. 895–899, 2009.
T. Apard, N. Bigorre, P. Cronier, F. Duteille, P. Bizot, and P. Massin, “Two-stage reconstruction of post-traumatic segmental tibia bone loss with nailing,” Orthopaedics and Traumatology: Surgery and Research, vol. 96, no. 5, pp. 549–553, 2010.
G. Schmidmaier, S. Herrmann, J. Green et al., “Quantitative assessment of growth factors in reaming aspirate, iliac crest, and platelet preparation,” Bone, vol. 39, no. 5, pp. 1156–1163, 2006